By David P. Piñero · Miguel J. Maldonado‑López · Ainhoa Molina‑Martin · Noelia García‑Sánchez · María L. Ramón · José L. Rincón · Alfredo Holgueras · Juan F. Arenillas · Álvaro Planchuelo‑Gómez · Luis Leal‑Vega · María Begoña Coco‑Martín
Abstract
Conclusions A 3-week visual training program based on the use of Gabor patches after bilateral implantation of trifocal diffractive IOLs may be beneficial for optimising the visual function, with neural changes associated suggesting an acceleration of neuroadaptation.
Trial registration ClinicalTrials.gov, NCT04985097. Registered 02 August 2021, https:// clini caltr ials. gov/ (NCT04 985097).
1. Introduction
Crystalline lens extraction with implantation of a multifocal intraocular lens (IOL) has been shown to be a safe and efficacious option to provide a complete visual restoration in patients undergoing cataract surgery [1] and for presbyopia compensation in patients with clear lens [2]. However, visual disturbances, especially under scotopic conditions, are still one of the main concerns of this type of implants [3–5].
These include suboptimal visual acuity, decreased contrast sensitivity, and perception of photic phenomena, such as haloes or glare, that can lead to high levels of patient dissatisfaction [6] and in the most severe cases to the need for IOL explantation [7]. Excluding the presence of tear film instability, IOL decentration or posterior capsular opacification, these visual disturbances are mainly related to the neuroadaptation to the optical behaviour of the implant [8]. This process has been shown to be associated with increased activity in cortical areas involved in visual attention (frontoparietal circuits), learning and cognitive control (cingulate), and task goal-oriented behaviour in the early postoperative period (caudate), with normalisation six months after surgery [9, 10]. There is then a brain activity regularisation towards a non-effort pattern [9, 10]. In some cases, this neuroadaptation can fail leading to visual dissatisfaction and complaints in which other brain areas might be involved, such as corticostriatal loops that contribute to the interpretation of ambiguous visual scenes [10].
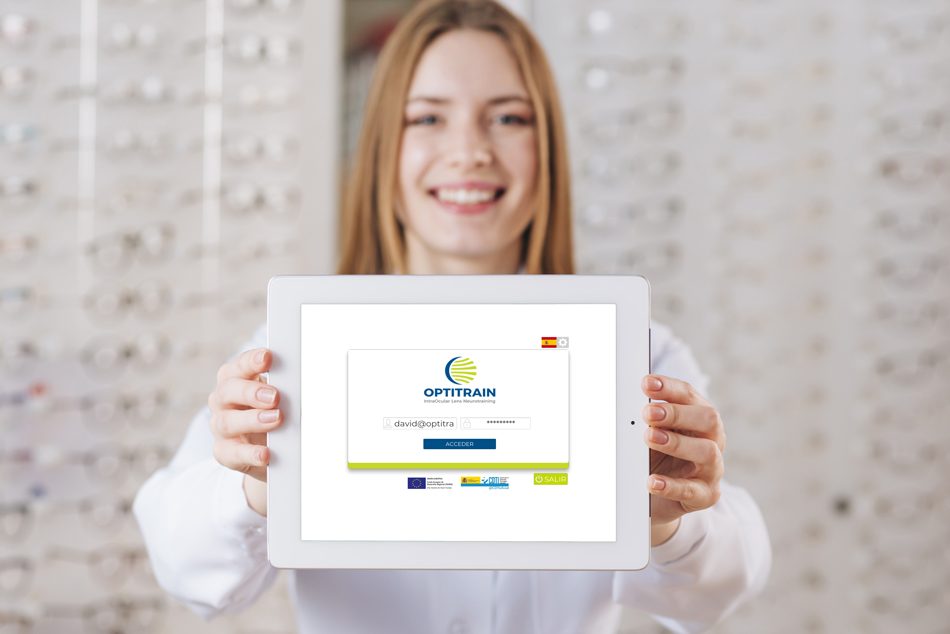
Some studies have shown that the visual function can be improved in patients implanted with multifocal IOLs by performing a well-oriented visual training program, suggesting the potential benefit of this approach for promoting or accelerating neuroadaptation [8, 11–13]. Kaymak et al. [12] reported the first results of a computer-based visual training experience in patients implanted with multifocal IOLs (diffractive bifocal and apodised diffractive), using only one eye for the training and serving the untrained fellow eye as a control. They reported an improvement in different visual parameters in spite of the limitations of the visual rehabilitation program used that was not gamified and used sinusoidal gratings without a smooth transition in their edges [12]. It should be considered that although the use of sinusoidal gratings with a neutral background can cause selective cortical responses for orientation and contrast [14], a stimulation of a specific channel is not achieved without an appropriate smoothing of the edges of the grating [15]. Recently, a new computerised game was developed to train the visual function of patients implanted with multifocal IOLs (OPTIcTRAIN®, Proconsi S.L., León, Spain), which is gamified and uses Gaussian-windowed sinewave gratings and exercises promoting the activation of frontoparietal circuits, cingulate, and caudate brain areas [11]. The preliminary results of the use of this game in patients implanted with trifocal IOLS are promising, providing significant improvements in distance and near contrast sensitivity [11].
Resting-state functional magnetic resonance imaging (rs-fMRI) is a safe and noninvasive technique that provides comprehensive and accurate data on brain anatomy, function and metabolism, making its incorporation into clinical studies highly recommended for assessing changes in functional connectivity produced by different therapies, including visual training [16]. This methodology has previously been applied in the field of vision for the general study of the various brain networks involved, such as the high-level visual network (HVN), the visuospatial network (VSN) or the primary visual network (PVN) [17], allowing comparison between healthy subjects and those with certain types of visual disorders. For example, Lu et al. [18] found a loss of functional correlation within the HVN and VSN by contrasting functional brain activity of 18 patients with anisometropic amblyopia against a sample of 18 age- and sexmatched healthy controls. In addition, rs-fMRI also makes it possible to visualise changes in the architecture of these networks in the same subject after a given treatment. This is the case of Halicka et al. [19], who evaluated the effects of 44 h of virtual realitybased active vision therapy over a period of 1.5 years on the visual cortex of an adult with anisometropic amblyopia. The use of rs-fMRI might be also useful to identify those changes occurring after the previously mentioned visual training in patients implanted with trifocal IOLs.
The aim of the current randomised placebo-controlled clinical trial was to evaluate the efficacy of this new visual training program for improving the visual function and minimising the perception of visual disturbances in a relevant sample of patients undergoing bilateral cataract surgery with the implantation of trifocal diffractive IOLs.
Furthermore, we aimed to assess functional and structural brain changes induced by therapy in these patients. On the one hand, a rs-fMRI substudy was performed on a small subsample of patients to confirm that the visual training program generated a differential impact on brain activity compared to the use of the placebo software. On the other hand, structural grey and white matter changes were assessed using morphometry parameters and diffusion MRI (dMRI) processing.